Approximately 76,000 pregnant women and 500,000 babies die from pre-eclampsia across the world every year. Women in developing countries are seven times more likely to suffer from the condition due to delayed diagnosis and a lack of access to hospitals.
Causes of pre-eclampsia are not entirely understood, but if left untreated it can lead to blood clots, organ failure, and death. Rapid, affordable, and accurate diagnostic tools are therefore essential in aiding treatment.
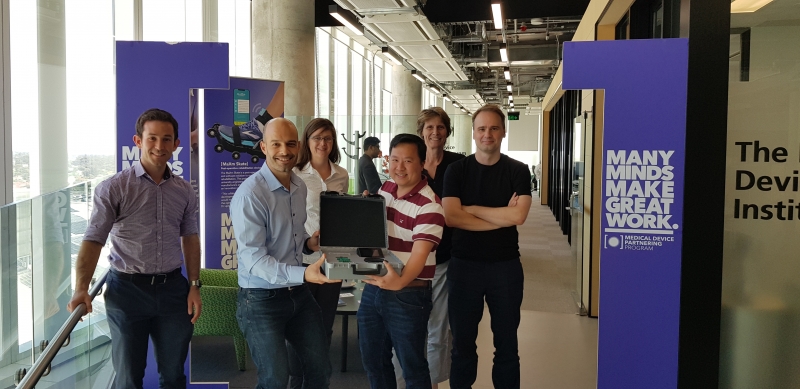
Now, with the help of the Medical Device Partnering Program, a portable diagnostic device being developed by Professor Benjamin Thierry, Dr Duy Tran and a team from the University of South Australia’s Future Industries Institute (UniSA FII) has shown it could pose a solution.
The affordable technology is already showing promising signs during early testing – a prototype developed by Dr Tran and PhD student Ms Thuy Pham has been successfully validated on four women with confirmed pre-eclampsia, and there are plans for further trials to be conducted in the Royal Womens Hospital (Melbourne) and Vietnam in the near future. The team’s new tool utilises a sensor developed at ANFF-SA, where Dr Tran has been harnessing the Node’s technical expertise and its lithography and sputtering equipment to fabricate and fine-tune the device.
The sensor works by placing a droplet of the patient’s blood onto a sensitive area of the device. This area contains receptors specific to pre-eclampsia biomarkers – if present, the biomarkers bind to the receptors and change the flow of electricity across the device. By monitoring these fluctuations in current, the presence and approximate quantity of pre-eclampsia biomarkers can be confirmed, allowing doctors to quickly react and mitigate the potentially life-threatening symptoms. Because the level of biomarkers can be detected, the severity of the condition can also be determined. With support from the ARC Centre for Bio-Nano Science (CBNS),
Dr Tran has built on local expertise to integrate his sensing technology within cost-effective and easy-to-operate diagnostic devices that can be operated with minimal training by nurses and other primary healthcare providers in regional and remote communities, both here in Australia and worldwide. The next generation of the device is currently being developed with the support of the Medical Device Partnership Program (MDPP) as a handheld analyser unit with single-use disposable sensing cartridges, anticipated to be manufactured for as little as two dollars.