Projects
We’ve considered well over 1,000 ideas for new medical devices since our establishment. We’ve completed over 210 collaborative workshops and 120 R&D projects.
Our clients come from a range of professions: surgeons wanting to improve the lives of patients; researchers needing assistance to get their research out of the labs and into the hands of end-users; industry from startups to established businesses who are diversifying their product line; and the everyday inventor who sees a problem and has an idea to solve it.
Projects have included special glasses that help frequent flyers and shift workers adjust their sleep cycle, a cancer-detecting probe that is improving surgical outcomes and a device to assist orthopedic surgeons when fixing bone fractures.
When Scott Blackburn injured himself badly in an accident, breaking both arms and his leg, he was surprised when the Ambulance arrived and treated him with a piece of cardboard.
Thinking there must be a better way, Scott established Fluoro Medical and created their first product, the CAS Splint. He then turned to the Medical Device Partnering Program (MDPP) for assistance to develop their new innovation.
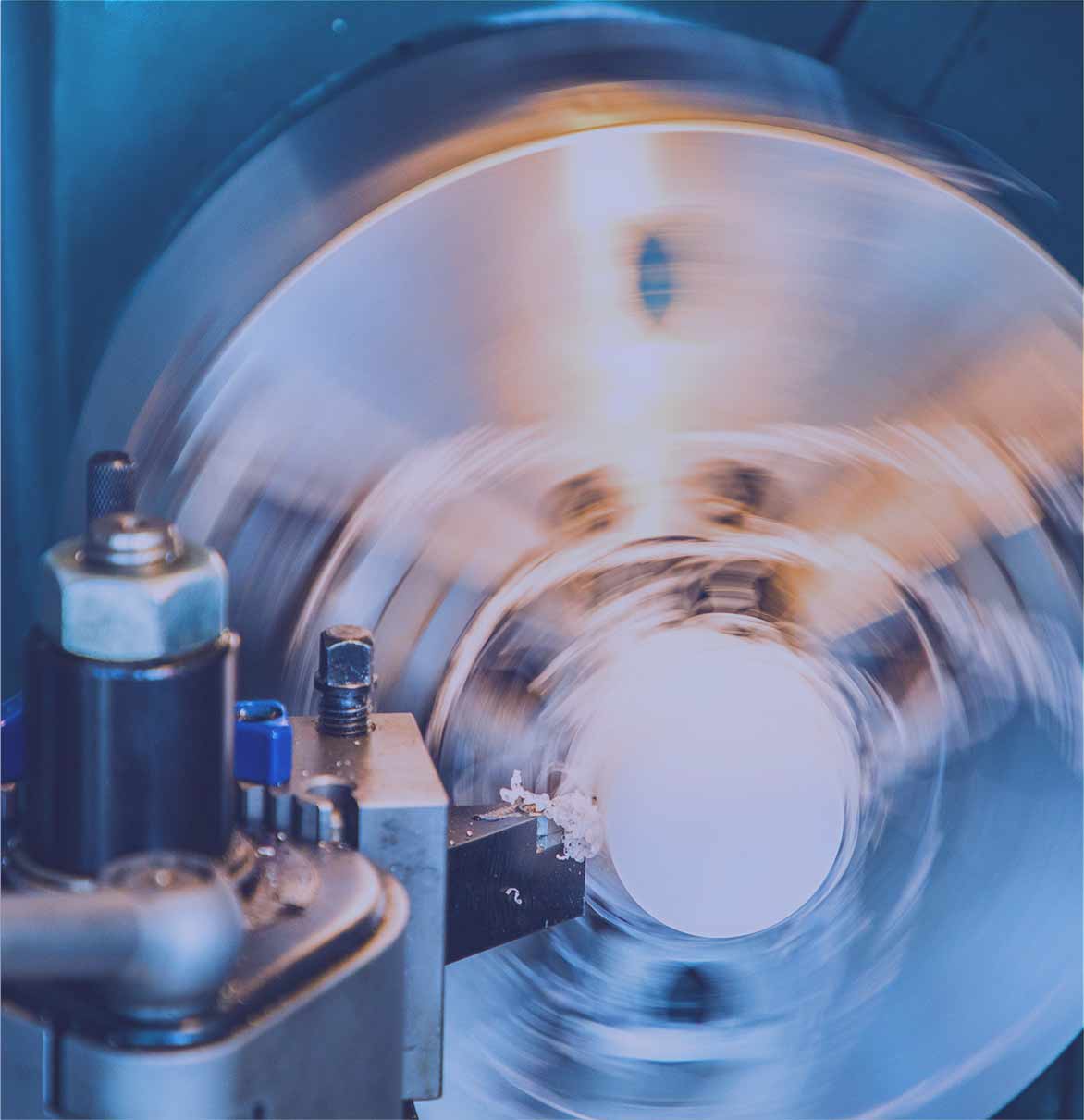
The CAS Splint is an innovative, foldable splint for fractured limbs that requires no training to use and does not have to be removed during x-rays.
The MDPP undertook an end-user trial and survey to validate the current design of the splint and made recommendations for design modifications. The MDPP also provided a market intelligence report to Fluoro Medical.
When ResMed, a world-leading connected health company, engaged with the Medical Device Partnering Program in 2010, they wanted to investigate the feasibility of measuring specific signals from the head or face of a patient with Obstructive Sleep Apnoea (OSA).
ResMed sought to develop a non-intrusive device to monitor the cardiac health of OSA patients which would enable the monitoring of health so treatment could be administered with greater insight.
Obstructive Sleep Apnoea (OSA) is a condition where a person's upper airway becomes blocked during sleep and impacts more than 936 million people worldwide. Not only does OSA impact sleep quality, but patients are at a greater risk of developing cardiovascular disease and other heart problems.
The MDPP project resulted in a collaboration between ResMed and Flinders University, with a PhD scholarship funded to further research and development in this area.
When Orthopaedic Surgeon, Dr Matthew Liptak started noticing inconsistent outcomes in the rehabilitation of his patients after total knee replacement, he decided to take things into his own hands.
He identified a gap in the market for a simple and effective device to encourage, motivate and monitor the rehabilitation of his patients post-surgery.
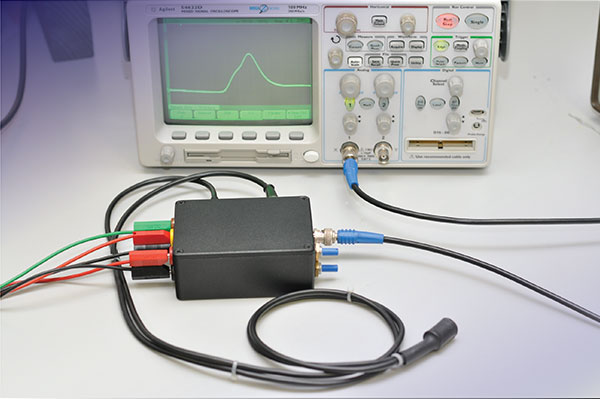
Dr Liptak first approached the MDPP in 2013 for assistance with the development of Maxm Skate, a skate-like device which straps to a patient’s foot. Whilst he had an initial prototype of the skate, he needed R&D assistance to develop a sensor which would record the user’s range of movement.
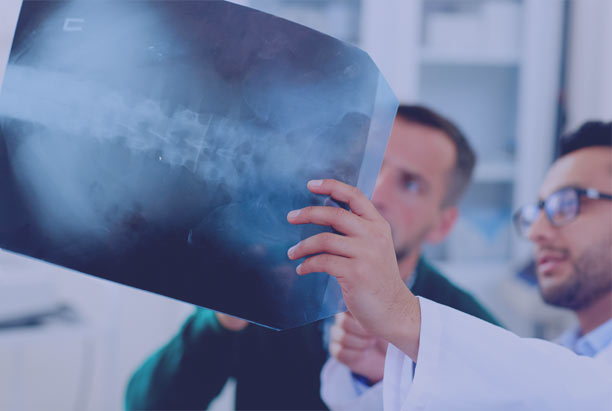
Detecting cancer is set to become safer and more accurate with the development of a new cancer-detecting probe.
The probe, an invention of University of South Australia researchers Professor Benjamin Thierry and Dr Aidan Cousins, provides a non-radioactive alternative to map how cancer has disseminated through the body.
Following initial bench-top testing of the device, the team first partnered with the MDPP in 2013, seeking out electronic engineering expertise and advice from end users and commercial experts.
Since 1987, world-renowned sleep psychologists, Professor Leon Lack and Dr Helen Wright from Flinders University, have studied the effects of light on the human body clock.
Their work focused on circadian rhythms, the fluctuations in biological process occurring on a 24-hour basis in the body. Research determined that exposure to bright light can normalize the timing of the rhythms and assist with the treatment of insomnia, winter depression, jet-lag and shift work disorder.
The result of this extensive body of work was Re-Timer, glasses proven to re-time one’s body clock. The glasses shine glowing green-blue light into the eye of the wearer to help manipulate their production of melatonin — the hormone the body uses to induce sleep.
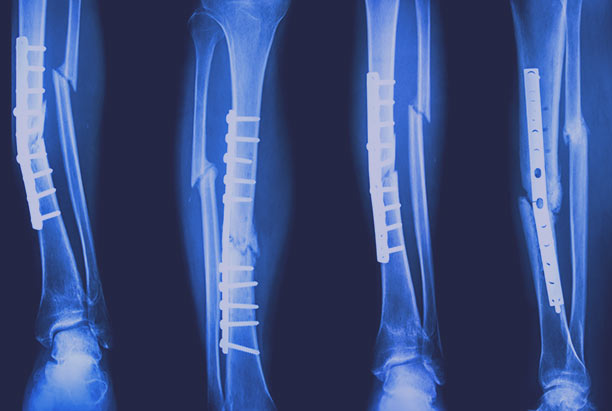
When Adelaide-based orthopaedics company, Austofix, wanted to fast track their invention to market, they partnered with the Medical Device Partnering Program to make it a reality.
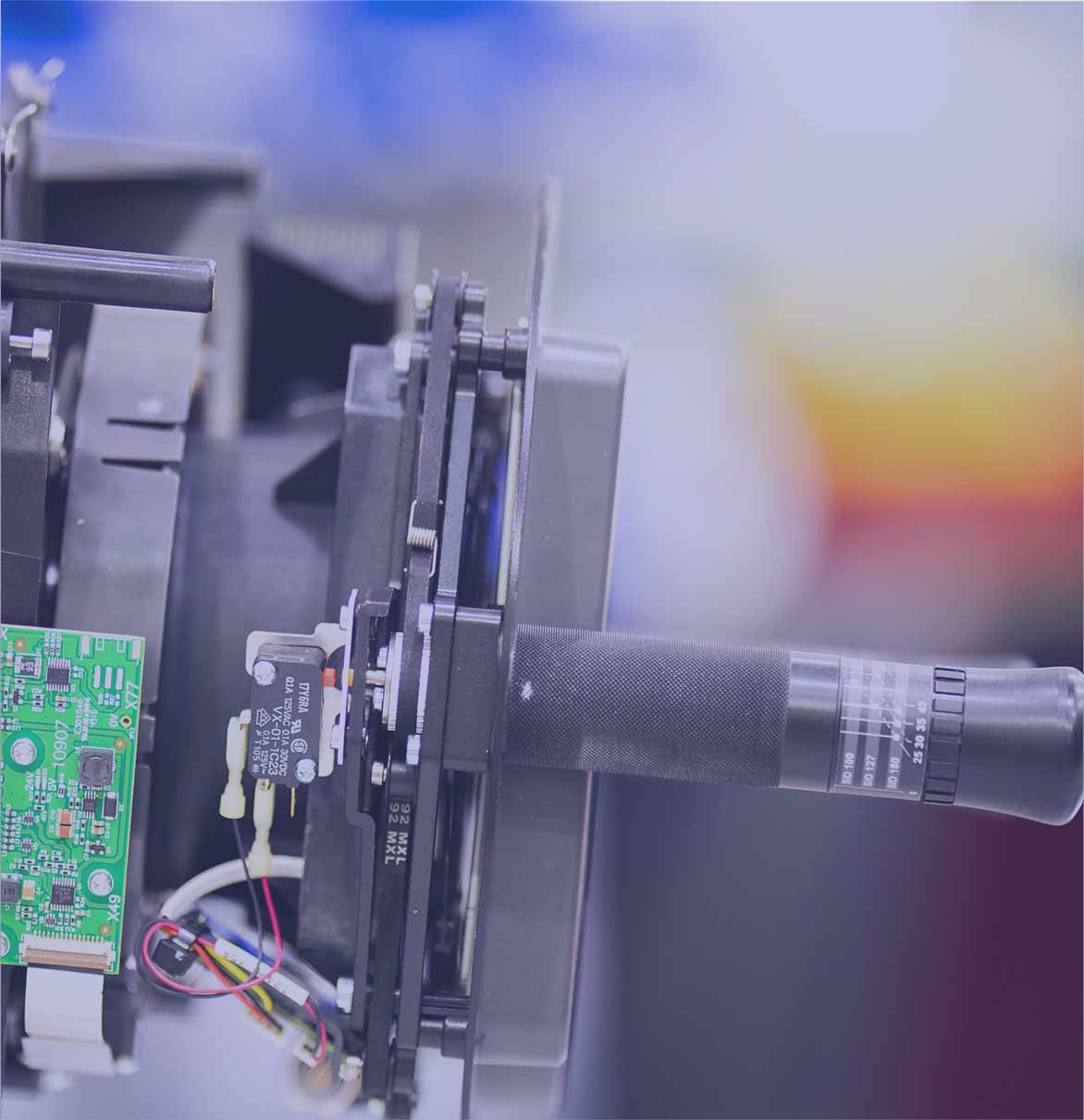
The Ezy-Aim Electronic Distal Targeting System, was developed to provide surgeons with ‘an extra pair of eyes’ when inserting nails and screws to repair broken bones.
The technology allows surgeons to accurately judge the location of the implant inside the bone, removing the need for multiple X-rays when fixing bone fractures.
MDPP supported University of Adelaide researchers to bring a new cancer-detecting probe to clinical trial.
The device – an optical fibre probe - identifies cancerous tissue in real time by measuring pH levels of tissue, assisting surgeons to precisely remove cancerous tissue while sparing the healthy tissue surrounding it.
Dr Erik Schartner and Professor Mark Hutchinson, who developed the concept, came to MDPP after conducting extensive lab based testing, “We were missing a prototype to demonstrate how the probe would function in an operating theatre. That is where the MDPP came in and we were very happy with their work.”
When Professor Matthew McDonald and Dr Peter Pedoulias had a revelation in the operating theatre about how spinal fusion surgery could be improved they turned to the Medical Device Partnering Program to make it a reality. Spinal fusion is a surgical procedure that corrects issues of the small bones of the spine by permanently connecting two or more vertebrae. This complex surgery is often the last resort to treat back problems and can cost around $46,700 per patient.
Helping patients and aged care residents to stand is all in a day’s work for many healthcare workers - but it comes at a cost, with nursing assistants suffering one of the highest rates of work-related musculoskeletal injuries.
A solution is now available thanks to a new medical device supported by the Medical Device Partnering Program, the ‘U-Stand Frame’. The lightweight and portable frame, an invention of Innovo Healthcare, is giving independence back to the patient, allowing them to control the timing, speed and mechanics of their sit-to- stand movement.
Page 2 of 2